Credentialing is a well known term among providers. Unlike few years before were a lot of physicians were able to run cash practices, these days they are finding that patients are persistent that they accept their insurance for payment. If providers don’t want to turn potential new patients away, they need to be in network with insurance companies.
The process of credentialing involves requesting and filling-up a lot of applications with insurance companies, sending them the filled applications, and a lot of follow up. We know that for a lot of providers this is a night mare as the application submitted rarely gets approved smoothly, and many find themselves redoing the applications, appealing enrollment rejections, and spending a lot of time on the phone holding with insurance companies.
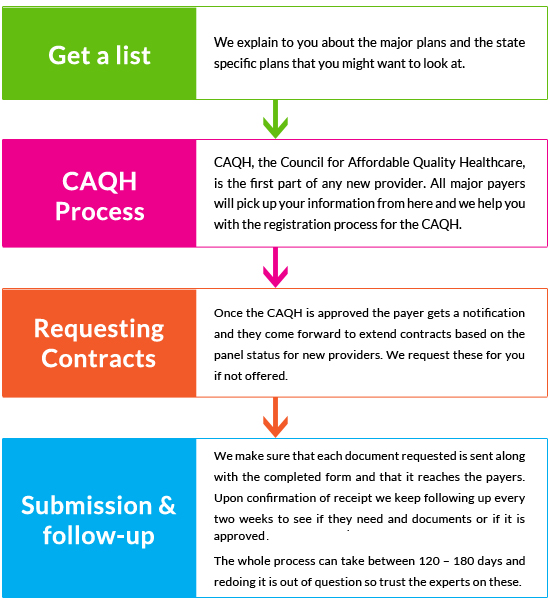
Here is how we help: